Presumed Ocular Histoplasmosis Syndrome in the Middle East: A Case Report
DOI:
https://doi.org/10.38179/ijcr.v2i1.24Keywords:
ocular, histoplasmosis, neovascularization, histospots, bevacizumab, presumed ocular histoplasmosis syndromeAbstract
Background:Presumed ocular histoplasmosis syndrome (POHS) occurs secondary to infection with Histoplasma Capsulatum (HC), which is an endemic organism in many tropical areas, especially in the United States. However, it has never been proven that HC directly causes POHS, hence the name presumed ocular histoplasmosis syndrome. Patients are usually asymptomatic, but some may present with blurring of central vision.
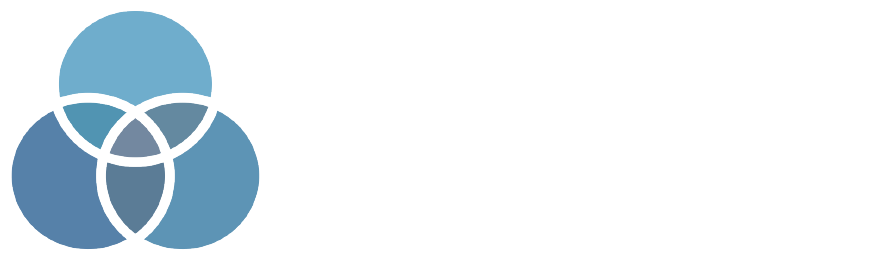
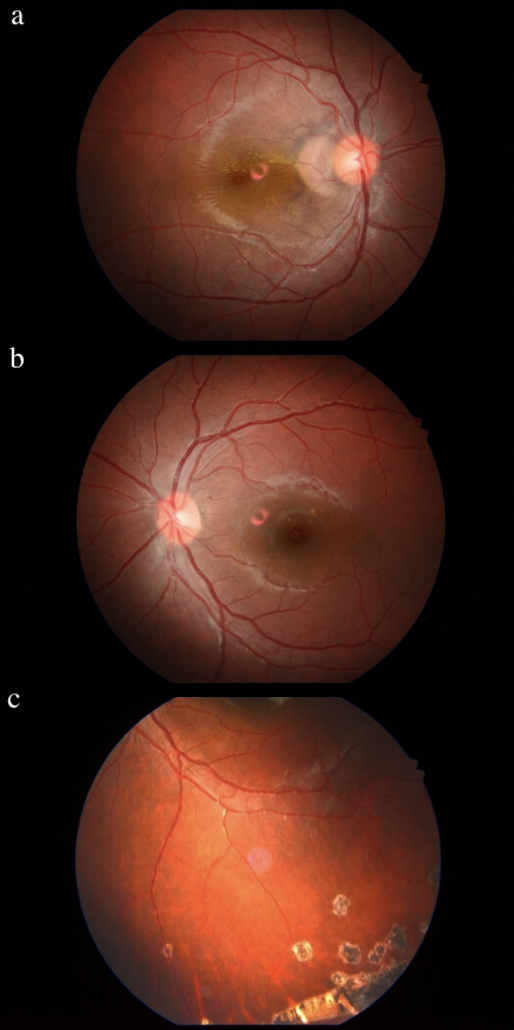
Case Report:A 15-year-old girl, previously healthy, presented with a 2-months history of visual disturbance of the right eye. On physical examination, the visual acuity of the left eye was 20/20 while the right eye was only seeing “hand motion”. Fundus exam of the right eye showed juxtapapillary infiltrates with serous macular detachment, and small retinal and choroidal lesions, while the left eye showed only some small retinal and choroidal lesions. Fluorescein angiography of both eyes showed evidence of chorioretinitis with probable choroidal neovascularization (CNV). The diagnosis of POHS was made and the patient was treated with bevacizumab injections. Follow-up was done clinically and through spectral domain optical coherence tomography (SD-OCT) and showed marked improvement at the level of the macular thickness and CNV.
Conclusion: Diagnosing POHS can be quite challenging, especially in cases coming from non-endemic areas. Our case emphasizes the importance of considering POHS in patients presenting with visual disturbance, even in these non-endemic areas, through a careful clinical evaluation and appropriate imaging modalities.
References
Nussenblatt R. Ocular Histoplasmosis. Uveitis. 2010;210-218. https://doi.org/10.1016/B978-1-4377-0667-3.00020-5
Tsai C, Tan C, Yang P, Chang K. Bevacizumab treatment for choroidal neovascularization in a patient with chorioretinopathy resembling presumed ocular histoplasmosis syndrome. Taiwan J Ophthalmol. 2012;2(4):144-147. https://doi.org/10.1016/j.tjo.2012.06.003
Mouzari Y, Atidi H, Jâafari D, Chekhchar M, Kriet M. Ocular Histoplasmosis: About A Case. Med Surg Ophthal Res. 2017 Dec 15; 1(2). doi: https://doi.org/10.31031/MSOR.2017.01.000506
Deshmukh S, Hawaibam S, Das D, Soibam R, Bhattacharjee H, Shrivastava R, Gupta K. Bilateral endogenous endophthalmitis in disseminated histoplasmosis secondary to immunosuppression: A rare case report. TNOA J Ophthalmic Sci Res. 2018;56(2):108. https://doi.org/10.4103/tjosr.tjosr_55_18
Asbury T. The status of presumed ocular histoplasmosis: including a report of a survey. Trans Am Ophthalmol Soc. 1966;64:371-400. PMID: 5964934; PMCID: PMC1310244
Diaz R, Sigler E, Rafieetary M, Calzada J. Ocular histoplasmosis syndrome. Surv Ophthalmol. 2015;60(4):279-295. doi: https://doi.org/10.1016/j.survophthal.2015.02.005. PMid:25841248
Oliver A, Ciulla TA, Comer GM. New and classic insights into presumed ocular histoplasmosis syndrome and its treatment. Curr Opin Ophthalmol. 2005;16(3):160-165. https://doi.org/10.1097/01.icu.0000161228.21797.d9. PMid:15870572
Sinha R, Raju S, Garg SP, Venkatesh P, Talwar D. Presumed ocular histoplasmosis syndrome in India. Ocul Immunol Inflamm. 2007;15(4):315-317. https://doi.org/10.1080/09273940701375428. PMid:17763129
Zaharova E, Sherman J. The use of SD-OCT in the differential diagnosis of dots, spots and other white retinal lesions. Eye Brain. 2011;3:69-80. Published 2011 Oct 25. https://doi.org/10.2147/EB.S23208 PMid:28539776 PMCid:PMC5436184
Ongkosuwito JV, Kortbeek LM, Van der Lelij A, et al. Aetiological study of the presumed ocular histoplasmosis syndrome in the Netherlands. Br J Ophthalmol. 1999;83(5):535-539. https://doi.org/10.1136/bjo.83.5.535 PMid:10216050 PMCid:PMC1723054
Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(7):807-825. https://doi.org/10.1086/521259. PMid:17806045
Yi X, Ogata N, Komada M, et al. Vascular endothelial growth factor expression in choroidal neovascularization in rats. Graefes Arch Clin Exp Ophthalmol. 1997;235(5):313-319. https://doi.org/10.1007/BF01739641. PMid:9176680
Yılmaz T, Dikci S, Genç O, Mutlu K. Multiple Intravitreal Ranibizumab Injections for Persistant Choroidal Neovascularization Associated with Presumed Ocular Histoplasmosis Syndrome. Turk J Ophthalmol. 2017 Apr;47(2):115-118. https://doi.org/10.4274/tjo.82956. PMid:28405488 PMCid:PMC5384118
Nielsen JS, Fick TA, Saggau DD, Barnes CH. Intravitreal anti-vascular endothelial growth factor therapy for choroidal neovascularization secondary to ocular histoplasmosis syndrome. Retina. 2012;32(3):468-472. https://doi.org/10.1097/IAE.0b013e318229b220/ PMid:21817958
Published
How to Cite
Issue
Section
Copyright (c) 2021 International Journal of Clinical Research

This work is licensed under a Creative Commons Attribution 4.0 International License.